CAPTAIN OF THE SHIP IN THE OPERATING ROOM
The Anesthesia Consultant
JUNE 6, 2025
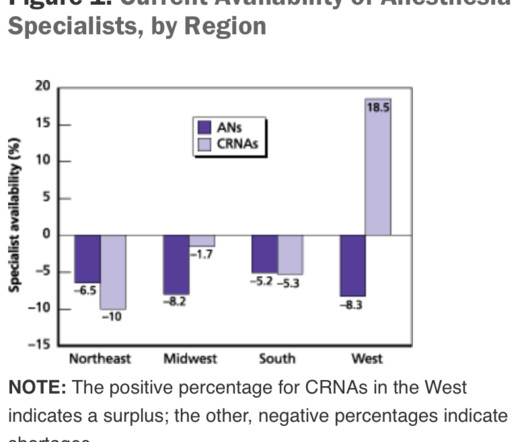
The operating room team today consists of multiple professionals working in collaboration, including the surgeon, the scrub tech, the circulating nurse, and the anesthesia MD or CRNA. Many surgeons chose to lord over the anesthesia attendings with verbal abuse and a condescending attitude.















Let's personalize your content