ANAPHYLAXIS DURING GENERAL ANAESTHESIA
Anaesthesia News
JUNE 18, 2025
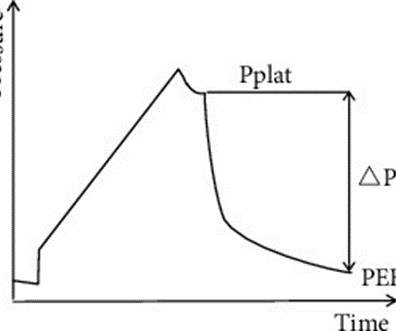
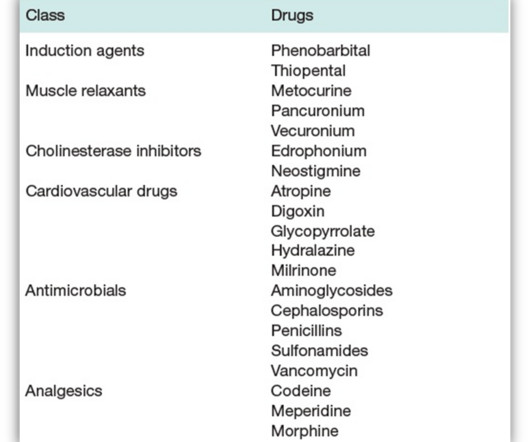
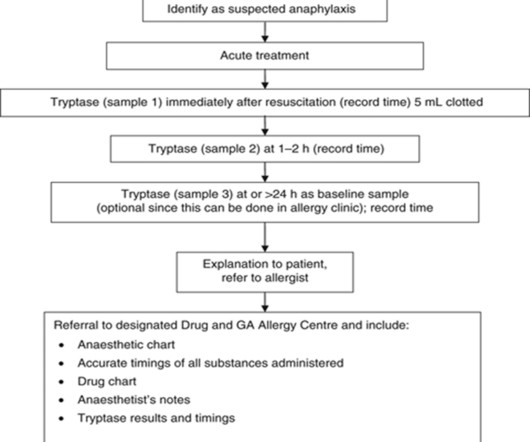
Death or permanent disability from anaphylaxis in anaesthesia may be avoidable if the reaction is recognised early and managed optimally. Recognition of anaphylaxis during anaesthesia is usually delayed because key features such as hypotension and bronchospasm more commonly have a different cause. If anaphylaxis is suspected during anaesthesia, it is the anaesthetist’s responsibility to ensure the patient is referred for investigation.
































Let's personalize your content