Battling Burnout in Nursing
The Circulating Life
JULY 16, 2025
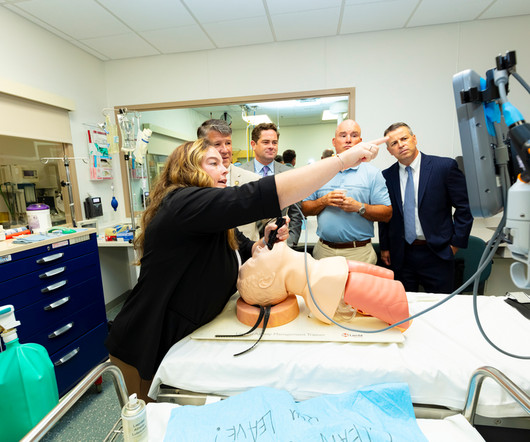
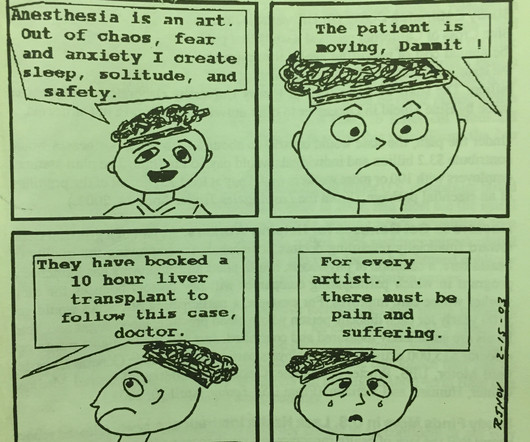
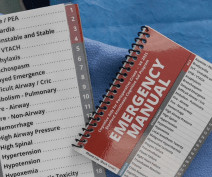
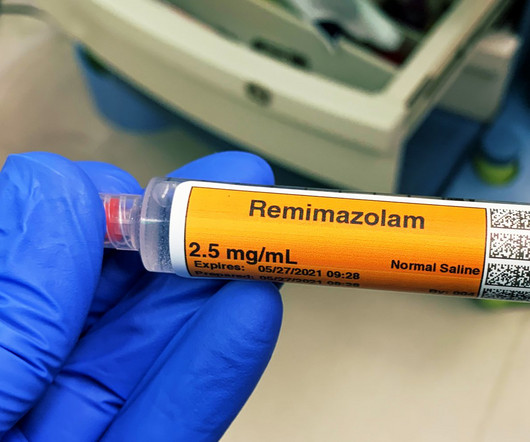
The operating room is a fast-paced, high-stakes environment where precision, teamwork, and vigilance are non-negotiable. Safe surgical care demands seamless collaboration between surgeons, nurses, techs, and anesthesia providers, so that we can achieve excellent outcomes. So How Do We Prevent Nurse Burnout?




































Let's personalize your content